Essential Businesses
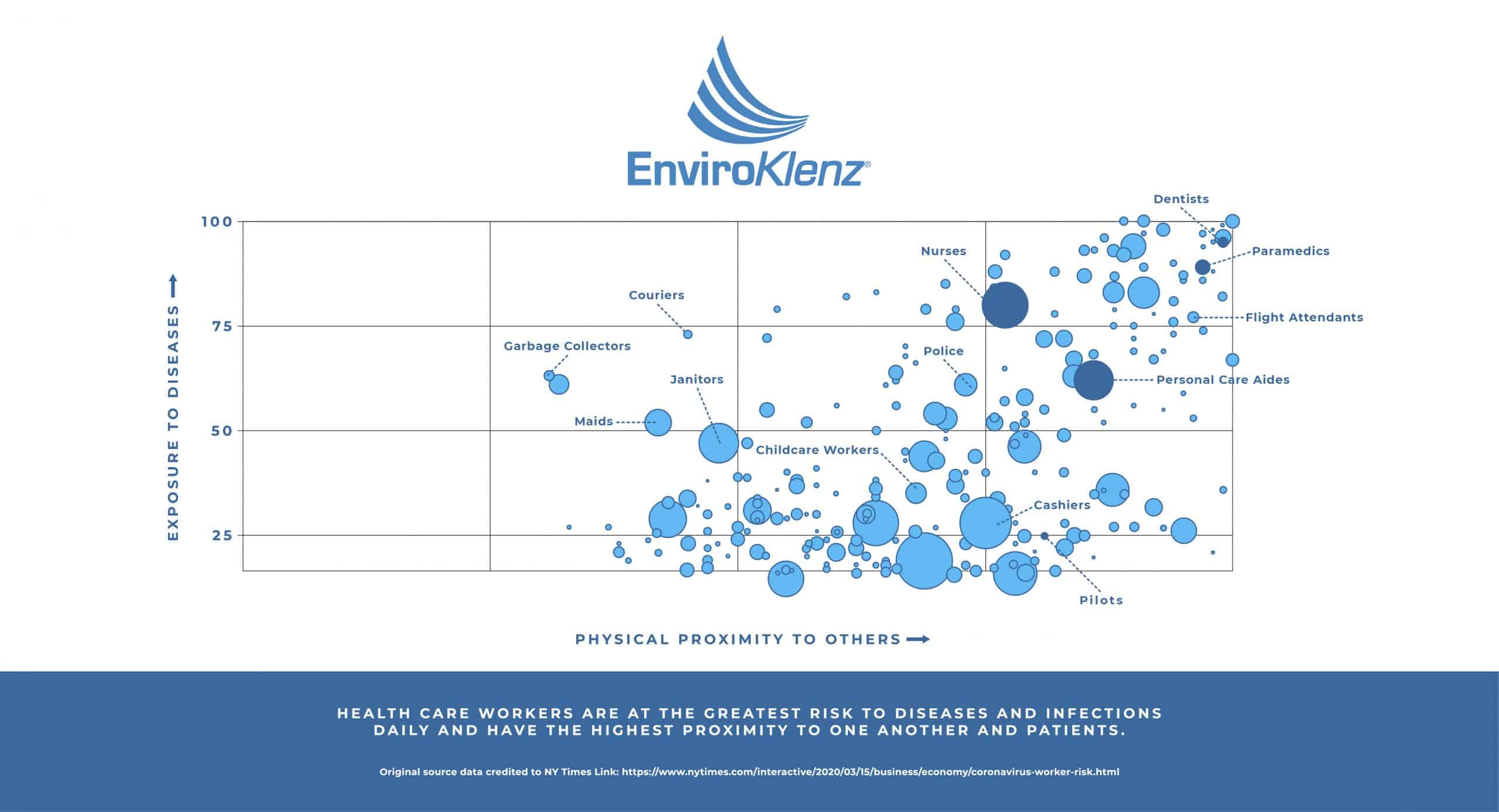
The outbreak of the pandemic Coronavirus disease (COVID-19), a highly contagious respiratory disease, has brought a new light to cleanliness practices and preventative mitigation methods that can be used in not only daily life, as well as in all medical settings. The development of this contagious disease has rapidly become a public health crisis that has spread exponentially throughout the world, which has called for many Countries to go on a public lockdown to fight to stop the spread. However, during this time many essential businesses must remain open during this pandemic, to give people access to the products and services that they need like grocery stores, public transportation, hospitals, and other medical facilities such as urgent care facilities, doctor’s offices, and dental practices. The widespread transmission of COVD-19 has become a risk not only for the everyday American but also to those who are having extreme levels of contact with people during this pandemic outbreak.
Understanding the Coronavirus Outbreak
Originating in Wuhan, China, the Coronavirus disease has steadily evolved into a global public health crisis, as it has spread aggressively to other parts of the world, including the United States. Coronaviruses are a type of virus that contains many different kinds, and some of these Coronaviruses will cause disease, like the recently identified COVID-19 infectious respiratory illness. John Hopkins Medicine stated the following about the spread of the new Coronavirus, “Researchers have identified that the new Coronavirus is spread through droplets that are released into the air when an infected person coughs or sneezes, and these droplets will generally not travel further than a few feet – and they will fall to the ground or other surfaces within a few seconds.”
As this new pandemic virus began its descent into the world, specifically public health, officials in the healthcare field have been extensively tracing the exact source of this newly introduced Coronavirus. The novel Coronavirus has been linked to a family of single-stranded RNA viruses known as Coronaviridae, a family of viruses that are known to be zoonotic and therefore transmitted from animals to humans, from findings published in the Virus Taxonomy. The strongest evidence has linked this novel Coronavirus to similar Coronavirus species found in bats, which confirms the zoonotic nature of this new cross-species Coronavirus that we are battling across the country, as well as throughout the world.
Technically, it is up to state and cities to redeem which retailers are essential or not, but all locales have considered these as essential: supermarkets and grocery stores, big-box stores, pharmacies, convenience stores, garbage collection, healthcare operations, daycare centers, hardware stores, gas stations, banks, post offices, veterinary clinics and pet stores, agriculture, transportation, and others.
These businesses have to take extra safety and prevention measures to stay open and slow the spread, since they are an imperative piece of the COVID-19 emergency response to ensure public health, safety, and community well-being.
The CDC has published an interim guide for essential businesses to help prevent exposures to COVID-19 in the workplace. Employers should plan to respond on a flexible way and be prepared to change business plans as needed. According to the OSHA (Occupational Safety and Health Administration), employees will experience low (caution) or medium level of exposure at their jobs.
Dentists
Dental emergencies can arise frequently and will require treatment by a dental professional immediately. These dental emergencies still take place, even during a pandemic like COVID-19, which has been found by the American Association of Endodontists (AEE) and the Centers for Disease Control and Prevention (CDC) to be a potential health risks to dental professionals across the world. The progression and spread of this contagious respiratory disease have led to the American Dental Association to release new information handouts for dentist on the Coronavirus and strategies on how to prevent the transmission of this virus specifically in the dental health care setting.
The Coronavirus has been shown to survive in aerosols for hours and on surfaces for days, and thus the lifespan of this virus can be compromising to many environments, including dental offices, as the American Dental Association has highlighted in their ADA Coronavirus Handout published in February 2020. This collected information from the American Dental Association (ADA) and the Centers for Disease Control and Prevention (CDC), who they collected information from in their published handout, have both encouraged that because of the dangerous transmission risks to dental professionals, that all dental practices only provide emergency and other essential care to patients during this pandemic. Therefore, strongly suggesting that elective treatment and other elective dental work be postponed to minimize the risks levels for dental care workers to the pandemic COVID-19 virus, according to Dentistry Today.
Vetranary Hospitals
Little is known on how or if COVID-19 can affect animals. According to the American Veterinary Medical Association, pet owners should:
– Keep cats indoors, when possible, to prevent them from interacting with other animals or people
– Walk dogs on a leash
– Until more is known about the virus, those ill with COVID-19 should restrict contact with pets and other animals, just as you would restrict your contact with other people.
– There is no evidence that animals (pets and livestock) play a role in the spread of COVID-19;
– Routine testing of animals for COVID-19 is NOT recommended
To maximize staff’s safety, veterinary clinics are recommended by the American Veterinary Medical Association to follow the same procedures as any other essential business, with these specialized recommendations:
– Screening clients for exposure to the virus
– Use telemedicine whenever possible
– Delay elective procedures
– Enforce social distancing
– Use of PPE
Essential Retailers
Among essential businesses, banks are one of the few ones that remain open, considering the economic impact the COVID-19 has brought to millions of Americans. It is important that banks protect their employees, and shifting from a central headquarter operation to distributed work-from-home operation is essential. According to Bain & Comapany, this can be 90% successful, with the exception of some fraud, audit, and back-office operations that may still need to be in-office. Good health practices include, but are not limited to:
– a timely supply of hand sanitizers, cleaning equipment, masks, gloves, and plastic or glass screens;
– branches will need new protocols for traffic management, including selective closures, reduced opening hours, staggered access for customers, and by-appointment-only meetings.
How to prepare for the future? To go beyond the steps of protection, banks need to:
– Raise cash through tactical cost cuts, as appropriate
– Accelerate digital readiness by promoting mobile and Internet banking
– Get serious about new ways of working, such as working from home and keep teams engaged and physically separated.
Another essential business that has been highly impacted are pharmacies, a vital part of the healthcare system. According to CDC, pharmacy staff can minimize the risk of exposure to COVID-19 by following the principles of infection prevention and control and social distancing.
Pharmacies, like other essential businesses, are recommended by the CDC to:
– Advise staff who are sick to stay at home;
– Provide hand sanitizer on counters for customers and staff;
– Encourage all customers to submit prescription orders via telephone or electronically
– Avoid handling insurance cards
– Avoid touching objects that have been handled by customers
– Promote the use of self-serve checkout registers
– Limit the number of customers inside at any given time
– Close self-serve blood pressure units
Private Practices
As another vital part of the healthcare system, private practices have special recommendation from the CDC to prepare for the COVID-19 pandemic. If you own or work at a clinic, these are the extra recommendations and resources to follow:
– The CDC has provided printable resources to prepare your practice. You can download them here: https://www.cdc.gov/coronavirus/2019-ncov/hcp/preparedness-resources.html
– Know what patients are at higher risk
– Plan to provide more telemedicine appointments
– Stay informed and connected with your health department
– Access and restock supplies on a regular schedule
– Reschedule non-urgent appointments
– Prepare the waiting and patient rooms with supplies, place chairs 6ft. apart, remove shareable objects such as magazines
– Practices should post front-door signage requiring patients and visitors who are exhibiting any of the “person under investigation” (PUI) evaluation criteria (e.g., presenting symptoms, recent contacts, and/or travel history) to immediately notify facility personnel via telephone
– Limit staff exposure to suspected patients, with the exam room door kept closed
Urgent Care
Many Americans have turned to urgent care centers as a more convenient means of health care. The popularity of urgent cares has gone up tremendously over the last two decades. The services provided by urgent cares range from anything such as a fever or cold all the way to minor cuts and small fractures. However, the services of an urgent care facility do not usually contain the care and testing of a highly infectious virus such as COVID-19. The question is- are they up for the task?
The following are recommendations provided by the CDC for health care facilities:
-
Stay informed about the local COVID-19 situation. Know where to turn for reliable, up-to-date information in your local community. Monitor the CDC COVID-19 website and your state and local health department websitesexternal icon for the latest information.
-
Develop, or review, your facility’s emergency plan. A COVID-19 outbreak in your community could lead to staff absenteeism. Prepare alternative staffing plans to ensure as many of your facility’s staff are available as possible.
-
Establish relationships with key healthcare and public health partners in your community. Make sure you know about healthcare and public health emergency planning and response activities in your community. Learn about plans to manage patients, accept transfers, and share supplies. Review any memoranda of understanding (MOUs) with affiliates, your healthcare coalition, and other partners to provide support or assistance during emergencies.
Create an emergency contact list. Develop and continuously update emergency contact lists for key partners and ensure the lists are accessible in key locations in your facility. For example, know how to reach your local or state health department in an emergency.
Restaurants
The restaurant business has been one of the hardest hit during this time. While many other similar businesses such as retail were forced to close, restaurants were deemed essential and many have chose to stay open for delivery or take out. Restaurants are required to follow local guidelines in order to ensure the safety of its employees and customers. In most states, many locations are taking precautions for this by offering curbside pickup and marking off space on the floors to promote distance between customers. Many restaurants are also requiring their employees to wear masks when preparing food and changing gloves frequently.
Like any other business, it is important to send any employee experiencing flu like symptoms home. If a customer come in showing flu like symptoms it is important to make sure that you clean and sanitize the area to avoid any further contamination. It is also suggested that as the situation rapidly changes, it is important for restaurant owners to stay aware of local regulations.
Advanced Air Purification for Chemicals, Odors, and Pathogens
The spread of pathogens between humans falls into direct or indirect contact; through airborne transmission, contaminated object and surface contact, and food and drinking water contamination. These three routes of indirect spread are often the result of contamination by the spray of droplets during coughing and sneezing, which can facilitate the spread of an infectious disease. Aerosolized droplets from humans range in size from .6 microns to over 1000 microns, collected from research published in the Characterizations of Particle Size Distribution of the Droplets Exhaled by Sneeze publication. Thus, the threat of exposure to an airborne pathogen can be potentially more significant, especially in certain medical care facilities such as dental settings.
Additionally, Ultraviolet light (UV light) is a known method for the inactivation or reduction in viability of pathogens, according to the CDC’s Infection Control Guidelines. However, the correct wavelength and control measures must be considered to avoid damage to the skin and eyes, as many UV light wavelengths can produce dangerous wavelengths that will ultimately produce ozone – a dangerous byproduct – within the indoor air space, reported by the American Cancer Society. Many air purification devices contain these UV lights to enable the capability to deactivate these airborne pathogens within the air purification system, but unfortunately a vast majority of these UV lights used in air purifiers fall within these hazardous wavelength production ranges which allow for the creation of ozone byproducts in the air.
The EnviroKlenz UV System solves the dosage problems by placing the UV-C light before the HEPA filter which captures biological contaminants 0.3 microns and larger. The droplet size from coughing or sneezing humans is very broad, and a HEPA filter can capture the bulk of that particulate matter range. Integrating UV lamps within the air purification device allows for continual bathing of the collection site of the HEPA filter, which allows for the items collected on the surface of the HEPA filter to get a lengthened or even infinite residence time. In the EnviroKlenz Mobile Air System with UV lights, the pathogens are exposed to the UV-C light as long as the unit and its lights remain on in the air purification system.
This means that even though the UV lamp is relatively low intensity, given the airflow of the unit (approximately 80-250 cfm), the UV-C dosage required for destruction is created for the trapped pathogen because it will continue to be exposed to the UV-C radiation regardless of how quickly air is passing through the unit.

UV Mobile Air System


✓ Patented earth mineral technology works to attack VOCs and break them down on a compound level
✓ No chemicals or masking agents
✓ Will not release any chemicals back into your environment
✓ UVC lamps are continuously shining on the collected organisms with high effeciency of kill and destruction
Comments
Post a Comment